Optimal Dose for Platelet-Rich Plasma (PRP) & Bone Marrow Aspirate Concentrate (BMAC)
For Musculoskeletal, Orthopedics, and Sports Medicine Applications
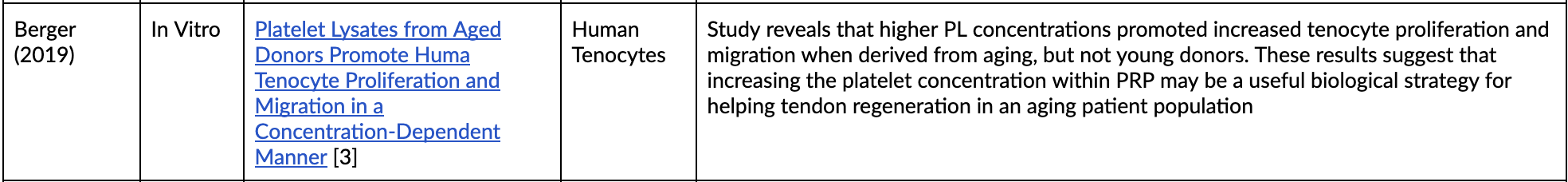
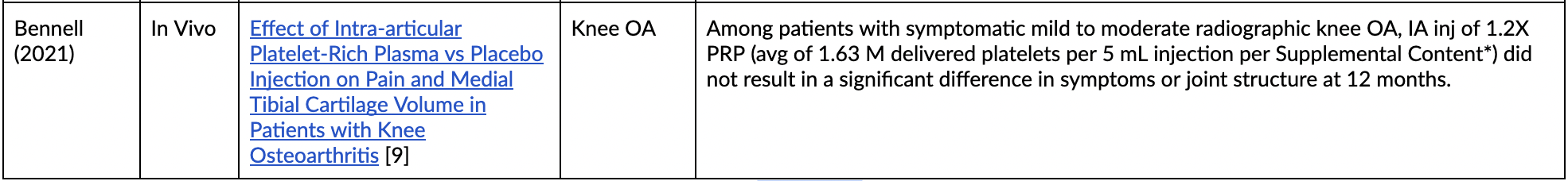
As demonstrated by the clinical studies summarized below, the clinical efficacy of PRP may be related to the total dose of platelets (PLTs) delivered per injection. Based on a level I RCT comparing PRP and HA for Knee OA (patients tested were reported with K-L Grade III), at least 10 Billion platelets must be delivered in an 8 mL aliquot of PRP [1]. Furthermore, in vitro, PRP Dose-Response studies corroborate this finding by demonstrating the increased metabolic activity, especially at the 1M plt/uL dose [6]. Conversely, studies utilizing underdosed PRP result in no clinical improvement to the patient [9].
This dose-dependent response extends to medicinal signaling cells (MSCs), with studies suggesting that at least 7800 MSCs to be delivered per mL to have enough benefit to avoid or postpone surgery [8].
PRP Dose-Response Studies
*Supplemental Content - click here
BM-MSC Dose-Response Studies
Citations
[1] Bansal, Himanshu, et al. “Platelet-Rich Plasma (PRP) in Osteoarthritis (OA) Knee: Correct Dose Critical for Long Term Clinical Efficacy.” Scientific Reports, vol. 11, no. 1, 2021, https://doi.org/10.1038/s41598-021-83025-2.
[2] Bec, Cécilia, et al. “A Retrospective Analysis of Characteristic Features of Responders and Impaired Patients to a Single Injection of Pure Platelet-Rich Plasma in Knee Osteoarthritis.” Journal of Clinical Medicine, vol. 10, no. 8, 2021, p. 1748., https://doi.org/10.3390/jcm10081748.
[3] Berger, D. R., et al. “Platelet Lysates from Aged Donors Promote Human Tenocyte Proliferation and Migration in a Concentration-Dependent Manner.” Bone & Joint Research, vol. 8, no. 1, 2019, pp. 32–40., https://doi.org/10.1302/2046-3758.81.bjr-2018-0164.r1.
[4] Centeno, Christopher J., et al. “A Dose Response Analysis of a Specific Bone Marrow Concentrate Treatment Protocol for Knee Osteoarthritis.” BMC Musculoskeletal Disorders, vol. 16, no. 1, 2015, https://doi.org/10.1186/s12891-015-0714-z.
[5] Gentile, Pietro, and Simone Garcovich. “Systematic Review—the Potential Implications of Different Platelet-Rich Plasma (PRP) Concentrations in Regenerative Medicine for Tissue Repair.” International Journal of Molecular Sciences, vol. 21, no. 16, 2020, p. 5702., https://doi.org/10.3390/ijms21165702.
[6] Giusti, Ilaria, et al. “Platelet Concentration in Platelet-Rich Plasma Affects Tenocyte Behavior in Vitro.” BioMed Research International, vol. 2014, 2014, pp. 1–12., https://doi.org/10.1155/2014/630870.
[7] Hahn, Olga, et al. “Dose-Dependent Effects of Platelet-Rich Plasma Powder on Chondrocytes in Vitro.” The American Journal of Sports Medicine, vol. 48, no. 7, 2020, pp. 1727–1734., https://doi.org/10.1177/0363546520911035.
[8] Hernigou, Philippe, et al. “Human Bone Marrow Mesenchymal Stem Cell Injection in Subchondral Lesions of Knee Osteoarthritis: A Prospective Randomized Study versus Contralateral Arthroplasty at a Mean Fifteen Year Follow-Up.” International Orthopaedics, vol. 45, no. 2, 2020, pp. 365–373., https://doi.org/10.1007/s00264-020-04571-4.
[9] Bennell, Kim L., et al. “Effect of Intra-Articular Platelet-Rich Plasma vs Placebo Injection on Pain and Medial Tibial Cartilage Volume in Patients with Knee Osteoarthritis.” JAMA, vol. 326, no. 20, 2021, p. 2021., https://doi.org/10.1001/jama.2021.19415. Direct Link to Supplemental Content
12/30/21