Blog: EmCyte vs. APEX – A Data-Driven Comparison of PRP Systems
With so many PRP systems on the market, identifying which system delivers truly therapeutic results—not just good marketing—is critical. Dr. Don Buford published “15 Data Points To Better Evaluate Platelet Rich Plasma Kits And Protocols” in the Journal of Orthopaedic Experience & Innovation. His framework outlines the essential information required to fully evaluate PRP kits and protocols before integrating them into practice.
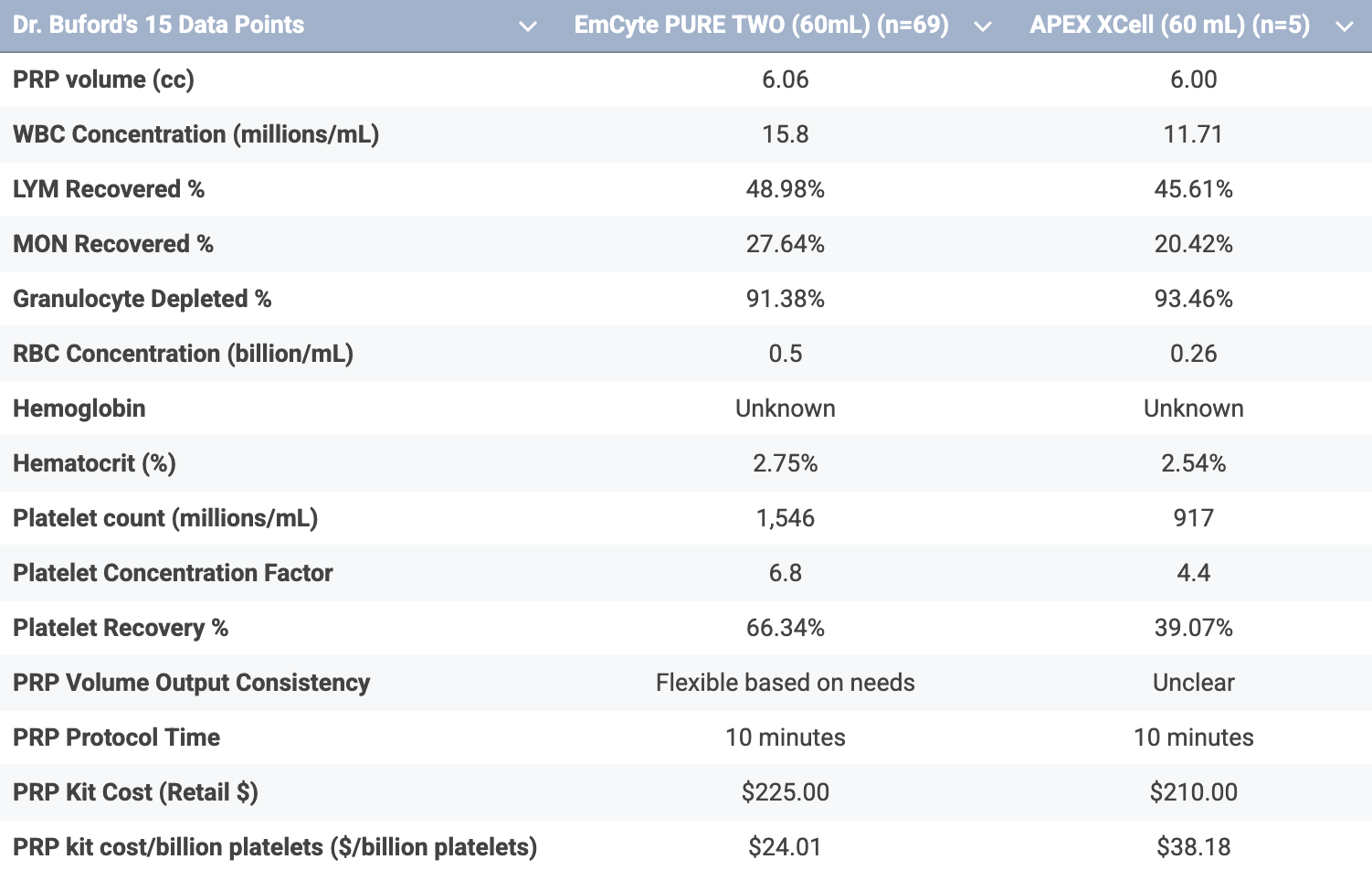
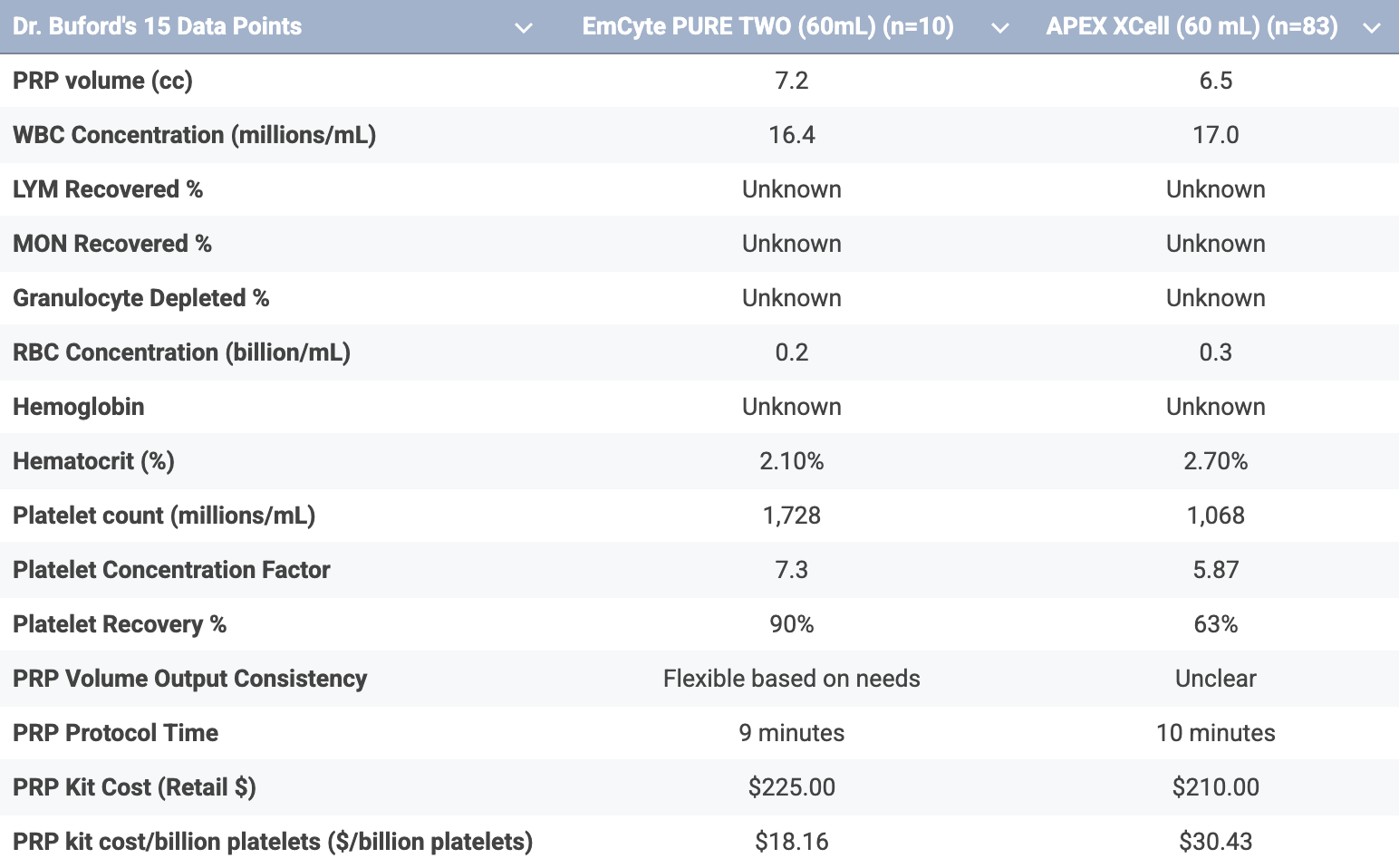
These 15 data points range from basic biological measures—such as platelet concentration, HCT %, and PRP volume—to practical considerations like protocol time, reproducibility, and cost per billion platelets.
We understand this is a lengthy, in-depth blog, but our goal is to leave you with three key takeaways when comparing these two commercial PRP kits. At PLYMOUTH MEDICAL, we use this framework to ensure every PRP system meets our performance, safety, and quality standards—and as always, we encourage you to do your own research.
Platelet Dose. Safety. Cost Effectiveness. These are the three factors our clients consistently identify as the most critical when selecting the best PRP kits for their patients and practice.
In this post, we’ll highlight how EmCyte PRP compares to APEX PRP across these key areas—specifically:
Safety
Efficacy & Efficiency
Therapeutic Dose Pricing Comparison
Complexity & Workflow
Customizability
By focusing on these critical benchmarks, clinicians can better understand not only the clinical impact of their PRP system but also the overall value it brings to their practice.
Safety
When preparing PRP, closed systems like EmCyte’s provide far greater protection against contamination compared to open systems. The closed design keeps the blood product sealed off from the external environment, while open systems leave samples exposed to room air and handling surfaces.
EmCyte PurePRP TWO (Closed System): Self-sealing ports keep the sample sterile and isolated from the environment, minimizing contamination risk.
APEX XCELL (Open System): Exposes the sample to room air and surfaces during preparation, creating a higher risk of microbial contamination.
APEX Manufacturer Contraindication:
We note that APEX themselves seem concerned with their open system, as their marketing brochures note the following under contraindications: “The XCELL PRP Platelet Concentrating System may be contraindicated when used in a non-sterile environment.”
Nota bene: This raises an important question—how realistic is it that every clinic using the APEX system is operating within a truly sterile environment, such as with the use of a laminar flow hood, as would be required to mitigate the risk of cross-contamination? The manufacturer’s own contraindication highlights a significant concern: by design, an open system inherently introduces contamination risk. If sterility can only be maintained under specialized conditions, the practicality and safety of routine clinical use should be carefully considered.
Efficacy & Efficiency
Platelet Dose
Platelet dose is a critical driver of PRP outcomes, as both concentration and the absolute number of platelets delivered determine therapeutic effect. Level 1 studies—such as Bansal et al. and Chu et al.—demonstrate that clinical efficacy in large joint osteoarthritis requires at least 10 billion platelets, whether achieved in a single treatment or across a short treatment series, as demonstrated in three sequential PRP injections of approximately 4.2 billion platelets each (~12.6 billion total platelets delivered across three injections). Importantly, this therapeutic threshold was achieved using PRP free of RBCs and WBCs, underscoring that both platelet quantity and purity are essential for optimal outcomes. More recent evidence supports a threshold of >5 billion platelets for chronic soft tissue pathologies.
Clinically, this raises an important consideration: systems producing PRP with fewer than 10 billion platelets per treatment may still reach effective total dosing—but only through multiple injections. This not only increases patient and clinic costs but also highlights the value of systems capable of delivering high-dose PRP in a single, efficient preparation.
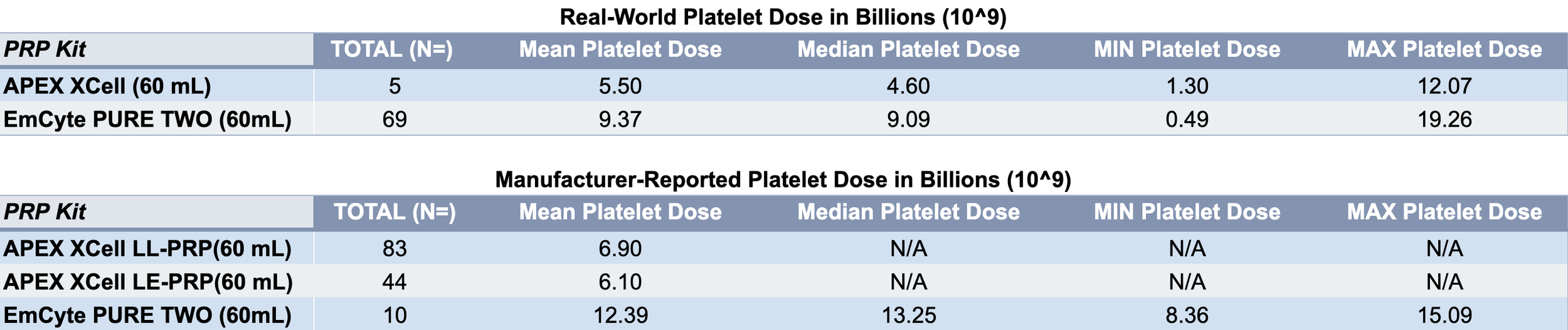
EmCyte PurePRP TWO (60mL): Manufacturer-reported data show an average of 12.39 billion platelets in a PRP sample from a 60 mL draw (n=10). Real-world data from PLYMOUTH MEDICAL’S Horiba Reporting Tool (n=69) demonstrated a mean platelet dose of 9.37 billion platelets.
APEX XCell (60 mL): According to APEX Biologix’s published data, the 60 mL Low-Leukocyte PRP configuration yields an average of 6.9 billion platelets per sample. More recent marketing data reported by Bioventus on file suggests even higher platelet doses beyond 10 billion platelets per sample yet no material changes were made to the kit design. Real-world Horiba data (n=5) demonstrated an average platelet dose of 5.5 billion platelets per sample.
Nota bene: When evaluating PRP systems, it is important to consider both manufacturer-reported performance and real-world clinical data. Together, these provide a more accurate picture of expected platelet yield and reproducibility in clinical practice.
Platelet Concentration Factor
Platelet concentration, or X-Factor, measures how enriched the PRP is relative to the patient’s baseline platelet count. This metric reflects how much the platelets are concentrated per unit volume and is directly influenced by dilution with plasma. However, the X-Factor alone does not account for total platelet dose or injectate volume, both of which are critical for therapeutic outcomes.
EmCyte PurePRP TWO (60mL): Provides a 7.3x platelet concentration in 7.2mL (n=10).
APEX XCell (60mL): Provides a 5.87x platelet concentration in 6.5mL for the Low-Leukocyte PRP configuration (n=83) and 5.3x for the Leukocyte-Enriched PRP configuration in 6.5mL (n=44).
Nota bene: This finding is particularly interesting, as leukocyte-enriched PRP would typically be expected to yield a higher X-Factor due to the additional platelet capture from the buffy coat along with all WBCs and some RBCs. Our team is noticing more sleight-of-hand marketing from manufacturers pointing to higher X-factor in small PRP volumes. Of course, it’s clear to most that espresso is more concentrated than an americano, but the true measure of a kit is whether it is able to provide flexible PRP volumes for various clinical needs such as CMC arthritis (1 mL) vs larger peripheral joint injections (4-8 mL). The EmCyte kit can provide flexible volumes of PRP and therefore flexible X-factor from 14x in 3.5cc PRP or 7x at 7cc PRP to 3.5x at 14cc PRP.
Platelet Recovery %
Platelet recovery percentage reflects the efficiency of a PRP system—how many platelets from the original whole blood draw (100%) are actually captured in the final product (x%). A higher recovery rate points to higher efficiency in recovering platelets from a whole blood sample, while lower recovery means a significant portion of platelets are not captured by the process.
EmCyte PurePRP TWO (60mL): Manufacturer-reported data (n=10) claim 90% platelet recovery, though it is important to consider the level of cellular contamination that may contribute to this value. Real-world Horiba data (n=69) demonstrated an average recovery of 66.34% platelet recovery.
APEX XCell (60 mL): Manufacturer-reported data claims an average of 63% platelet recovery for their 60 mL Low-Leukocyte PRP configuration (n=83) and 58% for the Leukocyte-Enriched PRP configuration (n=44). Real-world Horiba data (n=5) demonstrated an average recovery of 39.07% platelet recovery.
Nota bene: As with most manufacturer-driven marketing claims, discrepancies can exist between published performance data and independent clinical findings. Some manufacturers, including Bioventus, may report higher platelet recovery percentages (e.g., 84% platelet recovery rate) by allowing greater RBC and WBC contamination in the final PRP. While this may inflate recovery values, it can also increase inflammation and compromise product purity and therapeutic efficacy. For this reason, both recovery efficiency and cellular composition (aka PRP purity) should be evaluated together when comparing PRP systems.
PRP Volume (mL)
Total PRP yield is an important consideration for treatment coverage. Too small a volume limits injection options, while too large a volume with low concentration may dilute therapeutic potency.
EmCyte PurePRP TWO (60mL): Produces an average of 7.2 mL of PRP (n=10), with flexible customization ranging from 1 mL to 15 mL depending on clinical need.
APEX XCell (60 mL): A third-party independent evaluation reported an average output of 5.6 mL of PRP (n=12), while APEX Biologix’s own published data report an average PRP yield of 6.5 mL for their 60 mL Low-Leukocyte (n=83) and Leukocyte-Enriched PRP configuration (n=44).
Nota bene: Certain pathologies—particularly in soft tissue or spine injections—cannot tolerate higher injection volumes. For example, injecting 6 mL into an Achilles tendon could risk structural rupture, whereas a smaller, more concentrated 2 mL volume delivers therapeutic benefit safely and effectively. What’s important to consider is the system’s ability to titrate PRP volume to clinical needs without negatively impacting delivered platelet dose; having to leave PRP in the syringe rather than deploying the desired dose into the patient’s soft tissue or joint does not maximize treatment efficiency and may require multiple injections to reach therapeutic doses.
Hematocrit (HCT %)
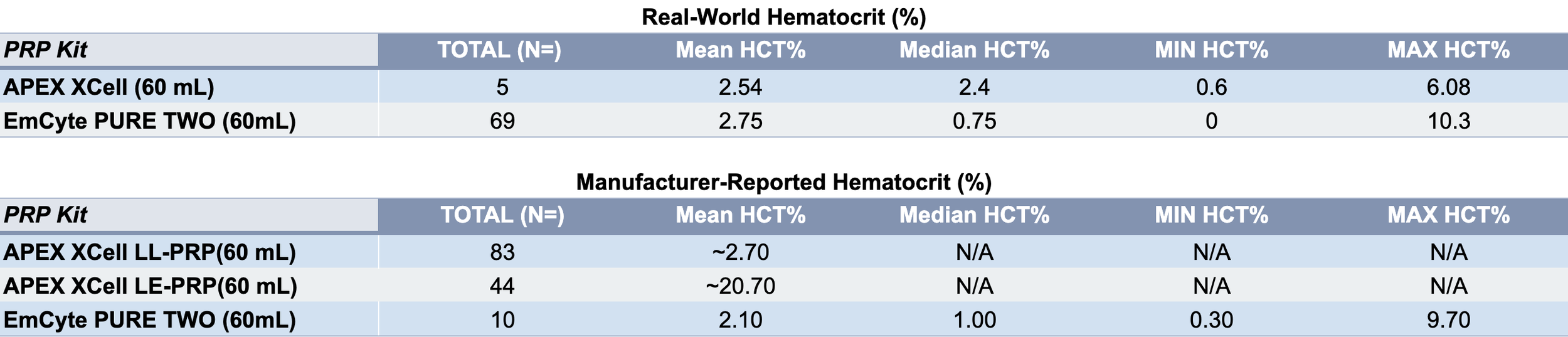
High RBC contamination can increase inflammation, pain, and limit the PRP’s effectiveness. The concepts of eryptosis and hemolysis have also been reported by renowned PhD scientists and orthobiologics clinicians, which hamper orthobiologics injections; namely, RBCs in PRP and BMAC injections seem to pose several deleterious effects on the tissue microenvironment, such as upregulating inflammation, oxidative stress, vasoconstriction, and impaired cell metabolism. Most PLYMOUTH MEDICAL clients, therefore, now aim for near-pure PRP (NP-PRP) with <2% hematocrit.
EmCyte PurePRP TWO (60mL): Produces an average HCT of 2.1% (n=10).
APEX XCell (60 mL): Produces an average HCT of 2.7% (n=83), which is higher than the NP-PRP target and may contribute to increased inflammation.
Nota bene: Notably, manufacturer-reported cell data often conveniently avoids providing HCT% data when platelet dosing is reported. RBC cells act as a roadblock for all cells in single-spin buffy coat systems like the APEX system, so capturing platelets in therapeutic doses often inevitably requires contaminating one’s PRP sample with RBCs and all WBCs.
Optimized Pricing
Evaluating PRP kits solely on upfront cost can be misleading. Per Dr. Buford’s 15-point evaluation system, the true metric of value is the cost per billion platelets delivered, which accounts for both kit price and platelet recovery %. This approach ensures that clinicians are paying for therapeutic efficacy, not just the kit. Assuming providers are aiming to achieve 10 billion platelets per injection, the therapeutic cost of deploying 10 Billion platelets should be compared across commercial PRP kits.
EmCyte PurePRP TWO (60mL): Cost per billion platelets ranges from $18.16 ($181.60 per 10B) based on manufacturer-reported dose of 12.39B and $24.01 ($240.10 per 10B), based on real-world Horiba data of 9.37B.
APEX XCell (60 mL): Cost per billion platelets ranges from $30.43 ($304.30 per 10B) based on manufacturer-reported data and $38.18 ($381.80 per 10B) based on real-world Horiba data of 5.50B.
Nota bene: In the spirit of comparing apples to apples, the therapeutic cost per billion platelets for each PRP kit should provide clinicians with much clearer pricing metrics in choosing the most cost-effective option without sacrificing the therapeutic dose. Of course, it is cheaper to purchase $80 PRP test tubes as shown in our RegenLab comparison post, but the costs of achieving a therapeutic 10B platelet dose with the latter kit far exceeds the use of more efficient kits such as EmCyte and APEX.
Complexity & Workflow
Protocol time reflects the efficiency and practicality of preparing PRP in a clinical setting. This includes centrifuge spin times, single- vs double-spin protocols, as well as the manipulation steps required to produce the final PRP product. Shorter, more streamlined workflows minimize staff time, potential human error and patient wait times, while maintaining consistency, streamlined workflows and reliability.
EmCyte PurePRP TWO (60mL): Total centrifuge time is 6 minutes across both spins, with 4 minutes of manipulation, for a total protocol time of 10 minutes.
APEX XCell (60 mL): A total workflow time of about 10 minutes.
Nota bene: While single-spin systems are often marketed as simpler alternatives, both single- and double-spin PRP protocols still require additional time for blood collection, manipulation, centrifuge acceleration and deceleration phases, which extend the overall workflow duration.
Customizability
Customizability is an important feature of PRP systems, allowing clinicians to tailor the PRP injectate volume and formulation to the patient’s condition and treatment goals in terms of WBC content. While most kits offer some level of adjustment, the precision and control over that customization can vary significantly. It is also important to note that across all systems, increasing platelet yield often comes at the cost of pulling in more RBCs and neutrophils, which may negatively impact outcomes as described above.
EmCyte PurePRP TWO (60mL): Offers broad flexibility, with PRP volumes ranging from 1 mL to 15+ mL. Protocols can be adjusted to capture different cellular components, allowing clinicians to produce neutrophil-rich PRP (NR-PRP) or neutrophil-poor PRP (NP-PRP) depending on clinical need.
APEX XCell (60 mL): Customization is limited. While operators can attempt to take more or less of the buffy coat, the separation is not clearly defined, and RBC contamination occurs regardless of technique. The manufacturer IFU calls for the production of 6 mL of final PRP volume. However, we are told users are able to create flexible PRP volumes starting at 2 mL and can dilute their PRP with PPP to expand volume and dilute concentration.
Nota bene: In our APEX vs EmCyte PRP comparison video, EmCyte PRP was prepared without neutrophils because Dr. Malanga and his team were opposed to using RBC- and neutrophil-rich PRP in joints and also tendons, for that matter. The EmCyte system, however, allows both NP-PRP and NR-PRP by adjusting how much of the neutrophil-rich layer is captured after a quick first spin. It is also important to note that kit comparisons should include the ability for the kit to target appropriate injectate volumes so that no platelets are left behind. Creating 6 mL of PRP may work for peripheral joints, but targeting APEX PRP for spine or smaller joints will require leaving PRP in the syringe and not deploy all platelets into the target structures.
Conclusion
Dr. Buford’s 15-point framework makes it clear: evaluating PRP systems requires looking beyond marketing claims and focusing on verifiable performance data. Short of arming oneself with a point-of-care cell counter, providers must consider both manufacturer-reported and real-world clinical data and analyze each kit to gain an accurate understanding of product consistency, purity, and therapeutic potential.
When compared head-to-head across these critical benchmarks, EmCyte consistently demonstrates superiority—not only in platelet yield and purity, but also in system safety. Its fully closed, sterile design minimizes contamination risk at every step, a distinction that becomes especially important given the inherent exposure risk associated with open systems like APEX.
It is clear to see across all 15 criteria that EmCyte offers a safer, higher-quality, and more clinically therapeutic PRP preparation. For physicians and patients alike, that translates to purer samples, greater dosing, and confidence that each treatment aligns with the evidence-based standards outlined in Dr. Buford’s framework.
Real-World Reported Data
Manufacturer-Reported Data
Testing Data Sources:
EmCyte PurePRP TWO (60mL): PLYMOUTH MEDICAL Quality Control testing
EmCyte PurePRP TWO (60mL): Comparison Testing of PurePRP II® 60mL and PURE TWO 60mL Platelet Concentrating Systems
APEX XCell (60 mL): PLYMOUTH MEDICAL Quality Control testing
APEX XCell (60 mL): Rapid Preparation of Low-Leukocyte and Leukocyte-Enriched Platelet-Rich Plasma with XCELL PRP
Citations
Buford D, et al. In my experience…15 data points to better evaluate platelet rich plasma kits and protocols. J Orthop Exp Innov. 2024;5(2). doi:10.60118/001c.118697
Bansal H, et al. Platelet-rich plasma (PRP) in osteoarthritis (OA) knee: Correct dose critical for long term clinical efficacy. Sci Rep. 2021;11:3971. doi:10.1038/s41598-021-83025-2
Patel S, et al. Comparison of conventional dose versus superdose platelet-rich plasma for knee osteoarthritis. Orthop J Sports Med. 2024. doi:10.1177/23259671241227863
Stephens N. Comparison testing of platelet concentrating systems: EmCyte PurePRP-SP vs APEX Biologix XCELL PRP. BioSciences Research Associates, Inc; 2019.
EmCyte Corporation. PurePRP GenesisCS (GS-Pure II) instruction for use. EmCyte Corporation; Rev. 4.
APEX Biologix. XCELL Platelet Concentrating System 60mL™ (SKU XC-PRP-60 / PN 90-001) Instructions for Use. Rev 2.7. APEX Biologix; September 2025.
PLYMOUTH MEDICAL. PRP Comparison: EmCyte PurePRP vs EmCyte SP PRP vs APEX Xcell PRP [Video]. YouTube. Published February 26, 2020.
Mandle RJ. Performance data: EmCyte vs Arthrex Harvest comparison. BioSciences Research Associates, Inc; April 2015.
Bioventus. Bioventus PRP.
Rosenthal R, et al. Rapid preparation of low-leukocyte and leukocyte-enriched platelet-rich plasma with XCELL PRP. APEX Biologix.
Stephens NA. Test Report: Emcyte PurePRP® II vs PURE TWO 60mL Platelet Concentrating Systems. Biofyl Scientific Research; February 12, 2024.
Everts, P. et al. Assessing clinical implications and perspectives of the pathophysiological effects of erythrocytes and plasma free hemoglobin in autologous biologics for use in musculoskeletal regenerative medicine therapies. A review. Regenerative therapy, 11. 2021;56–64. https://doi.org/10.1016/j.reth.2019.03.009
Chu J, et al. Intra-articular injections of platelet-rich plasma decrease pain and improve functional outcomes than sham saline in patients with knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2022;30(12):4063-4071. doi:10.1007/s00167-022-06887-7
11/2/2025