Blog: The Plasma Edition
Concentrated Plasma:
One thing PLYMOUTH MEDICAL has insisted upon when it comes to promoting products or devices used in the production of Orthobiologic treatments, is EVIDENCE. This is why we have never sold exosomes and perinatal products and why we introduced cell counting and encourage the use of very high dose PRP in line with and in support of better clinical evidence.
This is true, but, possibly with one exception: Concentrated Plasma. PLYMOUTH MEDICAL have been proponents of plasma concentration for many years. But why? The in-vitro data shows promise, but in-vivo clinical studies are few and far between and do not look good for concentrated plasma.
And it is not just PLYMOUTH MEDICAL that have been promoting this equipment: We have seen a lot of companies selling plasma concentration filters. This recent study from Showel et al describes a protocol for producing A2M-rich plasma from platelet-poor plasma using the same filter PLYMOUTH MEDICAL have been selling for a number of years. And we see other manufacturers - each claiming their filter is more efficient than the last, doing the same.
Understanding that plasma is approximately 92% water, the concept of filtering it to remove some of this water appears to make sense. Filtering increases the relative concentrations of a number of key large plasma proteins, including Alpha-2-Macroglobulin, fibrinogen and Albumin.
Some of these proteins have shown great potential benefit: On paper, A2M appears to be the front runner in terms of clinical benefit.
A2M can bind to and neutralize certain enzymes that break down cartilage. A2M may also help reduce harmful inflammatory responses in joints. Animal studies prove that A2M can postpone cartilage degeneration by inhibiting the majority of catabolic enzymes and cytokines, making it a potentially valuable osteoarthritis treatment. One of the other concentrated proteins in plasma is albumin which serves as a very versatile and biocompatible scaffolding material.
BUT…. In concentrating the beneficial large plasma proteins, we are also concentrating all of the other large plasma proteins: Fibrinogen for example. Fibrinogen has been shown in studies to exacerbate inflammatory joint disease through a mechanism linked to the integrin αMβ2 binding motif.
When a study is called “Plasma proteins take their toll on the joint in osteoarthritis”, perhaps we should be a bit more careful as to which proteins we are exposing the joints to.
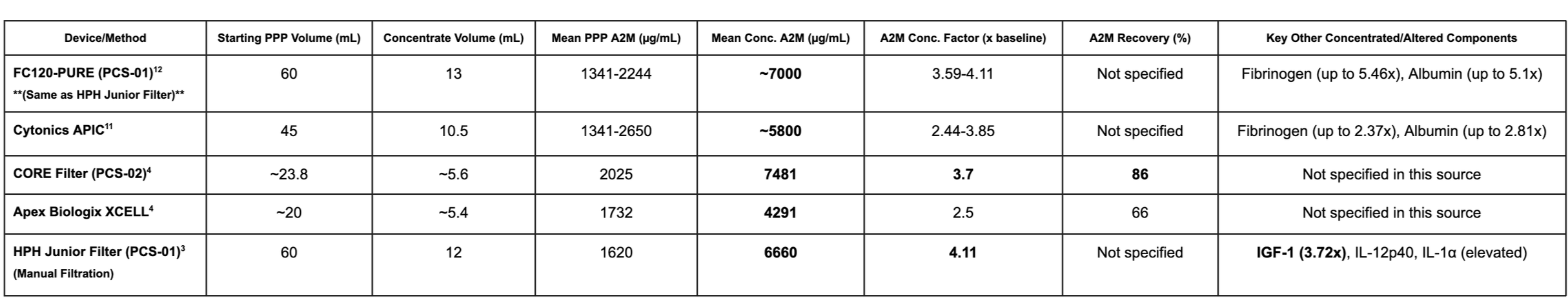
Here is a comparative table summarizing the A2M concentration and efficiency of various plasma concentrating devices, along with details on their performance:
Comparative Analysis of A2M Concentrating Devices
Note: Normal blood levels of A2M typically range from 1,000 to 3,000 µg/mL (or 1.5-1.8 mg/mL or ~2 mg/mL).
So where does that leave us?
Insufficient Clinical Evidence
The most glaring issue facing A2M therapy is the lack of robust clinical data. There are limited data on clinical efficacy and current studies show only modest improvements. Research demonstrates that Alpha-2-macroglobulin treatment resulted in modest improvement in knee pain and function at 6-week follow-up. Even more concerning, Alpha-2-Macroglobulin was not significantly better than (low-dose) regular PRP for knee arthritis symptoms, raising questions about whether the additional workflow complexity and cost are justified.
Most current evidence comes from animal studies rather than human trials. Results of animal experiments prove that the A2M can postpone cartilage degeneration, but translating these findings to human patients requires extensive clinical validation that simply doesn't exist yet.
Technical and Logistical Challenges & A Lack of Standardization
Extracting and concentrating A2M requires expensive equipment and a certain level of expertise, making it less accessible than PRP. Furthermore, the lack of point of care A2M testing, dosing and standardization makes it nearly impossible to compare results across studies or ensure consistent patient outcomes. This variability undermines confidence in the therapy and makes it difficult to establish evidence-based treatment protocols.
Cost-Benefit Concerns
Given that A2M shows only comparable efficacy to established treatments like PRP and corticosteroids, the additional cost and complexity may not be justified. The equipment and training requirements significantly increase treatment expenses without documented proportional improvements in patient outcomes.
Conclusion
Our mission has always been to provide our clients and their patients with protocols that pass the rigors of peer review and are anchored in clinical evidence. While we wait for the evidence on Plasma concentrates to catch up with efficacy and dosing clearly correlated by indication and level of pathology, we will continue to put our weight behind high dose Platelet-Rich Plasma which is low in neutrophils and RBCs for the treatment of Osteoarthritis (OA) and soft tissue injury as well as suggesting Platelet-Poor Plasma for the treatment of acute muscle injuries. While concentrated plasma does seem to play a positive role in interventional Orthobiologics and some components of plasma, when dehydrated, are clearly providing some relief for patients with OA further clinical research is definitely warranted with larger patient cohorts. PLYMOUTH MEDICAL will be investing in this space in order to fully understand the potential of this autologous treatment across several MSK conditions.
Citations
Mandle R. Alpha 2-Macroglobulin Concentrators: EmCyte-FC120 PURE vs Cytonics APIC. Performance report. November 2, 2015. Bio Sciences Research Associates, Inc.; 2015. Available here.
08/08/2025